Abstract
CONTEXT
Medications represent a major cause of harm and are costly for hospitalized patients, but more is known about these issues in large academic hospitals than in smaller hospitals.
OBJECTIVE
To assess the incidence of adverse drug events (ADEs) in six community hospitals.
DESIGN
Multicenter, retrospective cohort study.
SETTING
Six Massachusetts community hospitals with 100 to 300 beds.
PATIENTS
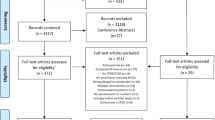
From 109,641 adult patients hospitalized from January 2005 through August 2006, a random sample of 1,200 patients was drawn, 200 per site.
MAIN OUTCOME MEASURES
ADEs and preventable ADEs.
METHODS
Presence of an ADE was evaluated using an adaptation of a trigger instrument developed by the Institute for Health Care Improvement. Independent reviewers classified events by preventability, severity, and potential for preventability by computerized physician order entry (CPOE).
RESULTS
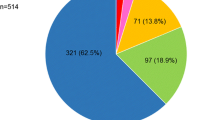
A total of 180 ADEs occurred in 141 patients (rate, 15.0/100 admissions). Overall, 75% were preventable. ADEs were rated as serious in 49.4% and life threatening in 11.7%. Patients with ADEs were older (mean age, 74.6 years, p < 0.001), more often female (60.3%, p = 0.61), and more often Caucasian (96.5%, p < 0.001) than patients without ADEs. Of the preventable ADEs, 81.5% were judged potentially preventable by CPOE.
CONCLUSIONS
The incidence of ADEs in these community hospital admissions was high, and most ADEs were preventable, mostly through CPOE. These data suggest that CPOE may be beneficial in this setting.
Similar content being viewed by others
References
Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324(6):370–6.
Bates DW, Leape LL, Cullen DJ, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. Jama. 1998;280(15):1311–6.
Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. Jama. 1995;274(1):29–34.
Kaushal R, Shojania KG, Bates DW. Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review. Arch Intern Med. 2003;163(12):1409–16.
Bates DW, Teich JM, Lee J, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc. 1999;6(4):313–21.
Moore RT. Health Care Priorities for the 2007-2008 Legistlative Session. Joint Committee on Health Care Financing. 2006.
http://www.masstech.org/ehealth/update/index_8_15_06.html. 2009.
Morimoto T, Gandhi TK, Seger AC, Hsieh TC, Bates DW. Adverse drug events and medication errors: detection and classification methods. Qual Saf Health Care. 2004;13(4):306–14.
Bates DW, Boyle DL, Vander Vliet MB, Schneider J, Leape L. Relationship between medication errors and adverse drug events. J Gen Intern Med. 1995;10(4):199–205.
Mann K, Rothschild JM, Keohane CA, Chu JA, Bates DW. Adverse drug events and medication errors in psychiatry: methodological issues regarding identification and classification. World J Biol Psychiatry. 2008;9(1):24–33.
Kaushal R, Jaggi T, Walsh K, Fortescue EB, Bates DW. Pediatric medication errors: what do we know? What gaps remain? Ambul Pediatr. 2004;4(1):73–81.
Rozich JD, Haraden CR, Resar RK. Adverse drug event trigger tool: a practical methodology for measuring medication related harm. Qual Saf Health Care. 2003;12(3):194–200.
Kilbridge PM, Campbell UC, Cozart HB, Mojarrad MG. Automated surveillance for adverse drug events at a community hospital and an academic medical center. J Am Med Inform Assoc. 2006;13(4):372–7.
Peterson JF, Kuperman GJ, Shek C, Patel M, Avorn J, Bates DW. Guided prescription of psychotropic medications for geriatric inpatients. Arch Intern Med. 2005;165(7):802–7.
Chertow GM, Lee J, Kuperman GJ, et al. Guided medication dosing for inpatients with renal insufficiency. Jama. 2001;286(22):2839–44.
Wolfstadt JI, Gurwitz JH, Field TS, et al. The effect of computerized physician order entry with clinical decision support on the rates of adverse drug events: a systematic review. J Gen Intern Med. 2008;23(4):451–8.
Leape LL, Bates DW, Cullen DJ, et al. Systems analysis of adverse drug events. ADE Prevention Study Group. Jama. 1995;274(1):35–43.
Schiff GD, Klass D, Peterson J, Shah G, Bates DW. Linking laboratory and pharmacy: opportunities for reducing errors and improving care. Arch Intern Med. 2003;163(8):893–900.
Hulse RK, Clark SJ, Jackson JC, Warner HR, Gardner RM. Computerized medication monitoring system. Am J Hosp Pharm. 1976;33(10):1061–4.
Kaushal R, Jha AK, Franz C, et al. Return on investment for a computerized physician order entry system. J Am Med Inform Assoc. 2006;13(3):261–6.
Classen DC, Pestotnik SL, Evans RS, Lloyd JF, Burke JP. Adverse drug events in hospitalized patients. Excess length of stay, extra costs, and attributable mortality. Jama. 1997;277(4):301–6.
Bates DW, Spell N, Cullen DJ, et al. The costs of adverse drug events in hospitalized patients. Adverse Drug Events Prevention Study Group. Jama. 1997;277(4):307–11.
Resar RK, Rozich JD, Simmonds T, Haraden CR. A trigger tool to identify adverse events in the intensive care unit. Jt Comm J Qual Patient Saf. 2006;32(10):585–90.
Fortescue EB, Kaushal R, Landrigan CP, McKenna KJ, Clapp MD, Federico F, et al. Prioritizing strategies for preventing medication errors and adverse drug events in pediatric inpatients. Pediatrics 2003; 111(4 Pt 1):722–729.
Kaushal R, Bates DW, Landrigan C, McKenna KJ, Clapp MD, Federico F, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA 2001; 285(16):2114–2120.
Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA 1998; 280(15):1311–1316.
Acknowledgements
We thank Jason Lee, research assistant, for building the Access Database and the study nurses, Kris Martel-Waldrop, Cathy Foskett, Mary-Clare Hickey, Theresa McNeil, and Martha Vander Vliet, all RNs, for collecting data at the multiple study sites.
Conflict of Interest Disclosure Statements
The Massachusetts Technology Collaborative supported the study. They commented on its design, but were not involved in collection, management, analysis, or interpretation of the data. They did approve the manuscript. Dr. Bates had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Bates is a co-inventor on Patent No. 6029138 held by Brigham and Women’s Hospital on the use of decision support software for medical management, licensed to the Medicalis Corporation. He holds a minority equity position in the privately held company Medicalis, which develops web-based decision support for radiology test ordering, and serves as a consultant to Medicalis. He is a consultant for Cardinal Health, which makes intravenous drug delivery systems. Dr. Hug has received financial funding from the Freie Akademische Gesellschaft, the Walter and Margarethe Lichtenstein Fund, and the University Hospital in Basel, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was funded by the Massachusetts Technology Collaborative, which is not responsible for the contents of the manuscript.
Rights and permissions
About this article
Cite this article
Hug, B.L., Witkowski, D.J., Sox, C.M. et al. Adverse Drug Event Rates in Six Community Hospitals and the Potential Impact of Computerized Physician Order Entry for Prevention. J GEN INTERN MED 25, 31–38 (2010). https://doi.org/10.1007/s11606-009-1141-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-1141-3