Abstract
Objective
To examine whether oral care contributes to preventing ventilator-associated pneumonia (VAP) in ICU patients.
Design
Nonrandomized trial with historical controls.
Setting
A medical-surgical ICU in a university hospital.
Patients
1,666 mechanically ventilated patients admitted to the ICU.
Intervention
Oral care was provided to 1,252 patients who were admitted to the ICU during period between January 1997 and December 2002 (oral care group), while 414 patients who were admitted to the ICU during period between January1995 and December 1996 and who did not receive oral care served as historical controls (non-oral care group).
Measurements and results
Incidence of VAP(episodes of pneumonia per 1000 ventilator days) in the oral care group was significantly lower than that in the non-oral care group (3.9 vs 10.4). The relative risk of VAP in the oral care group compared to that in the non-oral care group was 0.37, with an attributable risk of −3.96%. Furthermore, length of stay in ICU before onset of VAP was greater in the oral care than in the non-oral care group (8.5 ± 4.6 vs 6.3 ± 7.5 days). However, no significant difference was observed in either duration of mechanical ventilation or length of stay between the groups (5.9 ± 10.8 vs 6.0 ± 8.8 days and 7.5 ± 11.5 vs 7.2 ± 9.5 days, respectively). Pseudomonoas aeruginosa was the most frequently detected bacteria in both groups. Number of potentially pathogenic bacteria in oral cavity was significantly reduced by single oral care procedure.
Conclusion
Oral care decreased the incidence of VAP in ICU patients.
Descriptor
Pulmonary nosocomial infection
Similar content being viewed by others
Introduction
Ventilator-associated pneumonia (VAP) is defined as hospital-acquired pneumonia occurring within 48 h after the initiation of mechanical ventilation with tracheal intubation. Development of VAP results in prolonged duration of mechanical ventilation, longer ICU stay, and increased health care costs [1]. It also increases the mortality of ICU patients to as high as 30–70% [2, 3]. Prevention of VAP is thus very important for the management of critically ill patients. Since mechanically ventilated patients cannot be fed orally, their salivary secretions decrease, and self-cleansing of the oral cavity is markedly reduced. As a result, oral cavity hygiene worsens, and the number of bacteria increases excessively, leading to bacterial colonization of the oropharynx. Several previous studies have reported a strong correlation between oropharyngeal bacterial colonization and presence of causative bacteria of VAP [4, 5, 6].
We hypothesized that oral hygiene and maintenance of cleanliness of the oral cavity, which is considered a reservoir of oropharyngeal colonization, contributes to prevention of VAP. We examined the effect of oral care through tooth brushing and washing on prevention of VAP without the risk of emergence of antibiotic-resistant bacteria.
A preliminary report of this research was presented at the Society of Critical Care Medicine 34th Critical Care Congress in January 2005 [7].
Materials and methods
Study design and patients
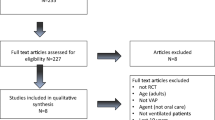
This non-randomized trial with historical controls was conducted at the medical-surgical ICU of a university hospital. Patients being admitted to the ICU during the period between January 1995 and December 2002 and receiving mechanical ventilation with tracheal intubation, regardless of age, sex, or underlying disease, were enrolled in this study. Of the 2,203 patients 1,252 patients required mechanical ventilation for 48 h or longer. Of these, four could not receive oral care, including one with intermaxillary anchorage after oral surgery, one with severe thermal burn complicated by respiratory tract burn, one with fulminant hepatitis and a serious hemorrhagic complication, and one with hemolytic uremic syndrome. All other patients were able to receiving oral care and accepted it with informed consent. Oral care was thus provided to 1,248 patients (the oral care group). On the other hand, of 637 patients admitted to the ICU between January 1995 and December 1996, 414 patients needed mechanical ventilation for more than 48 h but had not received oral care, and these patients served as historical controls (non-oral care group). Patient characteristics are shown in Table 1. There were no significant differences in age, sex, Acute Physiology and Chronic Health Evaluation II score on admission, or admission diagnosis between the two groups. During the study period an oral prosthesis was broken in two patients during oral care, but this did not affect the patient's condition. Fifteen patients who were randomly selected from the oral care group for examination of the effectiveness of the single oral care procedure were found to be representative of the study population for the following parameters: mean age, 53 vs. 51 years; male/female ratio 62/38 vs. 60/40 for studied patients vs. selected patients.
Intervention
The oral status of all patients in the oral care group was assessed at the time of admission to the ICU by a dentist or nurses working in the ICU, and an oral care nursing plan was established. Both the need for oral care and oral care methods were explained to patients who were scheduled to be admitted to ICU on an orientation held on the day before their ICU admission and to all conscious patients who were unexpectedly admitted to ICU upon their ICU admission. Informed consent to receive oral care was then obtained from all such patients. Oral care was provided three times daily or once in every nursing shift, according to the protocol shown below by a set of two members of the medical staff including a dentist and nurses who were trained to provide oral care.
-
1.
Check vital signs, then increase cuff pressure of the tracheal tube to 100 mmHg, and provide suction to remove oropharyngeal secretions in the oral cavity and portion of the trachea above the cuff.
-
2.
Position the patient's head to the side and have the patient open his/her mouth; observe inside the oral cavity and assess the condition of soft and hard tissues.
-
3.
Cleanse the oral cavity using a swab soaked in 20-fold diluted povidone-iodine gargle.
-
4.
Cleanse the oral cavity using a tooth brush carefully and rinse with 300 ml weakly acidic water (rinsing alone is performed for patients without teeth and those with bleeding tendency).
-
5.
Repeat cleansing of the oral cavity using a swab soaked in 20-fold diluted povidone-iodine gargle.
-
6.
Provide suction of the oral cavity and portion of the trachea above the cuff and restore the cuff pressure.
-
7.
Perform the entire procedure 3 times daily or once in every nursing shift.
Outcome measures
The incidence of VAP, time of onset of VAP, duration of mechanical ventilation, length of ICU stay, and causative bacteria were compared between the oral care and non-oral care groups. Potential confounding effects of all interventions for VAP prevention other than oral care performed during the study period (semi-recumbent patient positioning, use of an endotracheal tube with a suction port for subglottic secretion drainage, use of closed tracheal suction devices, and non-use of H2 blockers for stress ulcer prophylaxis) on the efficacy of oral care were examined by multivariate analysis, because these four co-interventions were preformed at different frequencies before and after the introduction of oral care. We also examined whether the single oral care procedure described here decreased the number of potentially pathogenic bacteria in the oral cavity.
Data collection and definitions
Age, sex, and diagnosis were recorded at the time of admission to the ICU. The patient's records including duration of mechanical ventilation and length of ICU stay were compiled in a database on a computer. Blood tests and chest radiographic examination were carried out every day throughout the patients ICU stay, and symptoms and signs of pneumonia were examined by more than one physician. VAP was suspected when a new, persistent, or progressive infiltrating shadow was observed on chest radiography at least 48 h after the start of mechanical ventilation, and when two of the following criteria were met: temperature higher than 38°C, leukocyte count higher than 10,000/mm3, or presence of purulent respiratory tract secretions. VAP was definitively diagnosed when a specimen of bronchoscopic tracheobronchial secretions [8] was subjected to semi-quantitative culture and a result of 1+ (corresponding to 104–105 cfu/mL on quantitative culture) or more was confirmed.
VAP detected within 48–96 h after the start of mechanical ventilation was defined as early-onset VAP (E-VAP), and VAP developing beyond 96 h after the start of mechanical ventilation was defined as late-onset VAP (L-VAP) [9].
Then during the period between July and December of 1997 we randomly selected 15 patients from the oral care group, regardless of whether they had developed VAP, and whether oral care was bacteriologically effective was examined for them. Specimens were collected from these selected patients during their ICU stay, once daily, before and after the single oral care procedure by wiping from the soft palate to the pharynx with a sterile swab. Among bacteria isolated from the harvested specimens, Pseudomonas aeruginosa, methicillin-resistant Staphylococcus aureus (MRSA), Candida, and other Gram-negative bacilli were semi-quantitatively cultured, and numbers of colonies before and after single oral care procedure were compared.
Statistics
Variables in both groups are expressed as the mean value ± SD. The incidence of VAP was calculated as episodes of pneumonia per 1000 ventilator days. Variables in both groups were compared using either 2 × 2 χ2 test or m × n χ2 test, or Fisher's test. Differences in mean values were tested using Student's t-test and confirmed by the Mann–Whitney U-test. The numbers of colonies before and after performing the oral care procedure were compared and examined by the two-sided Wilcoxon's t-test. In all tests a p-value less than 0.05 was considered statistically significant. All the statistical calculations and determinations of relative risk and attributable risk were performed using ystat2000.xls Windows version. Statistical correction of confounding effects was performed by logistic regression analysis using SPSS 12.0 for Windows (SPSS, Chicago, Ill., USA).
Results
VAP
The incidence of VAP (episodes of pneumonia per 1000 ventilator days) was significantly lower in the oral care group than in the non-oral care group (3.9 vs 10.4, p > 0.001). In a comparison of cumulative incidence of VAP by time of onset, the cumulative incidence of E-VAP was found to be markedly lower in the oral care group than in the non-oral care group. The cumulative incidence of L-VAP was also lower in the oral care group than in the non-oral care group, although not to a significant extent. Relative risk (RR) and attributable risk (AR) of oral care for VAP development as calculated from the results in these two groups were 0.37 (95% CI: 0.22–0.62) and −3.96, respectively. Examination of the incidence of VAP revealed that for E-VAP, RR was 0.08 (95% CI: 0.02–0.27) and AR −2.90, while for L-VAP, RR was 0.66 (95% CI: 0.34–1.28) and AR −1.06. These results indicated that the incidence of VAP in the oral care group was 0.37-fold that in the non-oral care group, and reduced to 3.96. The incidence of VAP was low in the oral care group, regardless of time of onset. In particular, in the case of E-VAP, it was one-tenth or less that observed in the non-oral care group.
In the oral care group the mean interval between the start of mechanical ventilation and onset of VAP was 8 days, while it was 6 days in the non-oral care group. Thus, the time elapsed to onset of VAP was significantly longer in the oral care group. However, comparison of duration of mechanical ventilation and length of ICU stay did not reveal significant differences between the two groups (Table 2). Effects of oral care and other interventions on the incidence of VAP were compared by multivariate analysis. Of the five variables tested, only oral care yielded a p value less than 0.05 (Table 3).
Bacteriological examination
The bacteria causative of VAP detected in this study are as follows:
-
Oral care (n = 29)
-
E-VAP: P. aeruginosa (n = 1), MRSA (n = 1), S. marcescens (n = 1)
-
L-VAP: P. aeruginosa (n = 9), MRSA (n = 6), Enterococcus faecali (n = 3), Acinetobacter. spp. (n = 2), Candida (n = 1), MSSAβ+ (n = 1), Burkholderia cepacia (n = 1), Enterobacter cloacae (n = 1), Neisseria spp. (n = 1), γ-streptococcus (n = 1)
-
Non-oral care (n = 26)
-
E-VAP: P. aeruginosa (n = 4), α-streptococcus (n = 2), Candida (n = 1), MSSAβ+ (n = 1), Enterobacter cloacae (n = 1), Haemophilus influenzae β- (n = 1), Stenotrophomonas maltophilia (n = 1), Citrobacter freundii (n = 1), Achromobacter xylosoxidans (n = 1)
-
L-VAP: P. aeruginosa (n = 5), MRSA (n = 4), Candida (n = 1), S. epidermidis (n = 1), GNF-GNB (n = 1), Neisseria. spp. (n = 1)
Among the causative bacteria isolated in both groups, P. aeruginosa was the most frequently observed, followed by MRSA and Candida.
All species of bacteria examined were significantly reduced after single oral care procedure (Fig. 1).

Pseudomonoas aeruginosa, methicillin-resistant Staphylococcus aureus (MRSA), and Candida isolated before and after the single oral care procedure
Discussion
The results of this study revealed that oral care can reduce the incidence of VAP in ICU patients as well as the risk of VAP development, and delay the onset of VAP. Examination of the incidence of VAP by time of onset revealed that the incidence of both E-VAP and L-VAP and particularly that of E-VAP was decreased.
E-VAP is generally understood to be caused by bacteria such as S. aureus, Streptococcus pneumoniae, and Haemophilus influenzae, while L-VAP is caused by antibiotic-resistant bacteria such as P. aeruginosa, MRSA, Acinetobacter, or fungi [10, 11, 12]. In this study causative bacteria of VAP isolated in the non-oral care group tended to be similar to those noted in previous reports, whereas in the oral care group E-VAP was caused by P. aeruginosa, MRSA, and Serratia marcescens. On the other hand, bacteria such as S. aureus, S. pneumoniae, and H. influenzae, which caused E-VAP in the non-oral care group, were not isolated in the oral care group. These results suggest that oral care has marked effects on bacteria causative of E-VAP and contributes to marked reduction of the incidence of E-VAP. In our study, P. aeruginosa and MRSA were the most frequently detected bacteria in both groups, and the risk of VAP development was markedly reduced by oral care.
The VAP prevention measures discussed to date can be broadly divided into two types. One is prevention of VAP by controlling aspiration of contaminated oropharyngeal secretions into the lower respiratory tract [13, 14, 15, 16],while the other is reduction in bacteria causative of VAP, including selective digestive decontamination (SDD) [17, 18, 19, 20] and chlorhexidine oral rinsing [21, 22]. It has been demonstrated using a benchtop model that it is difficult to completely prevent secretions from invading the airway through the space around the cuff of the tracheal tube [23]. There may be limitations to the efficacy of measures taken to prevent contaminant secretions from leaking into and invading the airways. Therefore, attempts have been directed toward elimination of bacteria in oropharyngeal secretions, on the assumption that the oropharynx is contaminated, and that secretions are aspirated to the lower respiratory tract. There are many reports in which the emergence of antibiotic-resistant bacteria with SDD has been discussed, although no clear conclusion has been reached regarding the usefulness of SDD for prevention of VAP [24, 25]. Furthermore, the effects of chlorhexidine oral rinsing on the oropharynx and the emergence of antibiotic-resistant bacteria caused by long-term performance of such rinsing have not been examined.
VAP prevention by oral care according to our protocol is similar to SDD and chlorhexidine oral rinsing in terms of approach taken against causative bacteria, but differs from these preventive methods in certain respects. First, SDD and chlorhexidine oral rinsing are performed to eliminate bacteria in the oropharynx on the assumption that the oropharynx is contaminated. However, we believe that oropharyngeal contamination is due to poor oral hygiene and that oral care consisting of tooth brushing and washing can decrease contamination in the oropharynx. Second, our method does not cause the emergence of antibiotic-resistant bacteria, because it does not aim at selective sterilization or bacteriostasis through a pharmacological effect, but at reducing the population of viable microbes mechanically. According to studies investigating the oral status of ICU patients, the amount of dental plaque increases as stay in the ICU is prolonged, leading to worsening of oral hygiene. Furthermore, a strong correlation has been found between colonization in dental plaque and development of nosocomial infections such as respiratory infections [5, 26].A large-scale study conducted in facilities for the elderly to examine the efficacy of oral care revealed that patients who received oral care, consisting mainly of tooth brushing, had a significantly lower incidence of pneumonia than those who did not receive oral care [6, 27]. Dental plaque, which is the major cause of oral contamination, is the thickest biofilm in the living body and cannot be eliminated by gargling or wiping [28]. Therefore, cleanliness of the oral cavity cannot be obtained by means other than mechanical cleaning including tooth brushing and washing. This study revealed that oral care performed according to our protocol reduces the number of potentially pathogenic bacteria in the oropharynx. Furthermore, the reduced incidence of VAP and delayed onset of VAP in the oral care group support the effectiveness of this oral care. However, since no significant differences were found in duration of mechanical ventilation or length of ICU stay between the oral care and the non-oral care groups, it may be true that in seriously ill patients, the factors affecting their outcome are not limited to VAP prevention.
There are several limitations to our study. Since patients admitted prior to the introduction of oral care were used as historical controls, there are several associated biases. Since the patients who participated in this study were admitted to the same ICU in the same hospital, their characteristics were nearly uniform. However, collection of a large number of samples necessary to assure the desired statistical power required a long study period. During the 8-year study period advances in treatment of underlying conditions and surgical techniques may have influenced the duration of mechanical ventilation and length of ICU stay. Although the methods used for patient management in the present study were basically unchanged during the 8-year study period, some of the various methods for VAP prevention published during that period (semi-recumbent patient positioning, use of an endotracheal tube with a suction port for subglottic secretion drainage, use of closed tracheal suction devices, and non-use of H2 blockers for stress ulcer prophylaxis) were introduced into our ICU (although not uniformly applied to all patients studied) [29, 30, 31, 32] and, in fact, differences in their frequency were noted before to after the introduction of oral care intervention. This change in co-interventions may potentially have had confounding effects on VAP prevention by oral care. To address this problem, confounding effects of these four co-interventions were eliminated by statistical correction by multivariate analysis.
Furthermore, the nursing staff changed during the study period although the supervising dentist and main staff did not change during the study period. Thus, in order to maintain consistent and adequate oral care technique, the nurses had to undergo periodic education and guidance by the supervising dentist. In this study the relationship between the bacteria detected in the oropharynx and colonization in the lower respiratory tract or bacteria causative of VAP was not examined in the same patients. In addition, although oral care was performed three times daily, we did not examine the duration of its efficacy, and the optimal frequency of oral care was thus not determined. Also, many of the patients studied were admitted to our ICU after elective surgery. In ICU patients of this kind, clinical condition might be less serious and VAP incidence lower than in trauma ICU patients and neurosurgical ICU patients. Effects of oral care in institutions with patients at higher risk for VAP remain to be examined.
This study, found that oral care consisting of tooth brushing and washing reduced the incidence and risk of VAP in ICU patients, and that it delayed the onset of VAP. To our knowledge, this study is the first on VAP prevention by oral care. Its findings warrant a large scale multi-center trial on the efficacy of oral care for VAP prevention.
Abbreviations
- VAP:
-
ventilator-associated pneumonia
- ICU:
-
intensive care unit
- SDD:
-
selective digestive decontamination
References
Fagon JY, Chastre J, Hance AJ, Montravers P, Novara A, Gibert C (1993) Nosocomial pneumonia in ventilated patients: a cohort study evaluating attributable mortality and hospital stay. Am J Med 94:281–288
Fagon JY, Chastre J, Domart Y, Trouillet JL, Pierre J, Darne C, Gibert C (1989) Nosocomial pneumonia in patients receiving continuous mechanical ventilation. Prospective analysis of 52 episodes with use of a protected specimen brush and quantitative culture techniques. Am Rev Respir Dis 139:877–884
George DL (1995) Epidemiology of nosocomial pneumonia in intensive care unit patients. Clin Chest Med 16:29–44
Fourrier F, Duvivier B, Boutigny H, Roussel-Delvallez M, Chopin C (1998) Colonization of dental plaque: a source of nosocomial infections in intensive care unit patients. Crit Care Med 26:301–308
Nardi G, Di Silvestre AD, De Monte A, Massarutti D, Proietti A, Grazia Troncon M, Lesa L, Zussino M (2001) Reduction in gram-positive pneumonia and antibiotic consumption following the use of a SDD protocol including nasal and oral mupirocin. Eur J Emerg Med 8:203–214
El-Solh AA, Pietrantoni C, Bhat A, Okada M, Zambon J, Aquilina A, Berbary E (2004) Colonization of dental plaques: a reservoir of respiratory pathogens for hospital-acquired pneumonia in institutionalized elders. Chest 126:1575–1582
Mori H, Hirasawa H, Oda S, Shiga H, Matsuda K, Nakamura M (2004) Oral care reduces incidence of ventilator-associated pneumonia in ICU population. Crit Care Med 32:A109
Woske H-J, Roding T, Schulz I, Lode H (2001) Ventilator-associated pneumonia in a surgical intensive careunit: epidemiology, etiology and comparison of three bronchoscopic methods for microbiological specimen sampling. Crit Care 5:167–173
Craven DE (2000) Epidemiology of ventilator-associated pneumonia. Chest 117:186–187
George DL, Falk PS, Wunderink RG, Leeper KV Jr, Meduri GU, Steere EL, Corbett CE, Mayhall CG (1998) Epidemiology of ventilator-acquired pneumonia based on protected bronchoscopic sampling. Am J Respir Crit Care Med 158:1839–1847
Neuhauser MM, Weinstein RA, Rydman R, Danziger LH, Karam G, Quinn JP (2003) Antibiotic resistance among gram-negative bacilli in US intensive care units: implications for fluoroquinolone use. JAMA 289:885–888
Robert R, Grollier G, Frat JP, Godet C, Adoun M, Fauchere JL, Dore P (2003) Colonization of lower respiratory tract with anaerobic bacteria in mechanically ventilated patients. Intensive Care Med 29:1062–1068
Drakulovic MB, Torres A, Bauer TT, Nicolas JM, Nogue S, Ferrer M (1999) Supine body position as a risk factor for nosocomial pneumonia in mechanically ventilated patients: a randomised trial. Lancet 354:1851–1858
Shorr AF, O'Malley PG (2001) Continuous subglottic suctioning for the prevention of ventilator-associated pneumonia : potential economic implications. Chest 119:228–235
Burns KE, Meade MO (2004) Noninvasive ventilation reduced duration of mechanical ventilation and ICU stay more than conventional weaning. Am J Respir Crit Care Med 168:70–76
Kearns PJ, Chin D, Mueller L, Wallace K, Jensen WA, Kirsch CM (2000) The incidence of ventilator-associated pneumonia and success in nutrient delivery with gastric versus small intestinal feeding: a randomized clinical trial. Crit Care Med 28:1742–1746
Collard HR, Saint S, Matthay MA (2003) Prevention of ventilator-associated pneumonia: an evidence-based systematic review. Ann Intern Med 138:494–501
Gastinne H, Wolff M, Delatour F, Faurisson F, Chevret S (1992) A controlled trial in intensive care units of selective decontamination of the digestive tract with nonabsorbable antibiotics. The French Study Group on Selective Decontamination of the Digestive Tract. N Engl J Med 326:594–599
Nardi G, Di Silvestre AD, De Monte A, Massarutti D, Proietti A, Grazia Troncon M, Lesa L, Zussino M (2001) Reduction in gram-positive pneumonia and antibiotic consumption following the use of a SDD protocol including nasal and oral mupirocin. Eur J Emerg Med. 8:203–214
Nieuwenhoven CA van, Buskens E, Bergmans DC, van Tiel FH, Ramsay G, Bonten MJ (2004) Oral decontamination is cost-saving in the prevention of ventilator-associated pneumonia in intensive care units. Crit Care Med 32:126–130
DeRiso AJ 2nd, Ladowski JS, Dillon TA, Justice JW, Peterson AC (1996) Chlorhexidine gluconate 0.12% oral rinse reduces the incidence of total nosocomial respiratory infection and nonprophylactic systemic antibiotic use in patients undergoing heart surgery. Chest 109:1556–1561
Genuit T, Bochicchio G, Napolitano LM, McCarter RJ, Roghman MC (2001) Prophylactic chlorhexidine oral rinse decreases ventilator-associated pneumonia in surgical ICU patients. Surg Infect (Larchmt)2:5–18
Young PJ, Rollinson M, Downward G, Henderson S (1997) Leakage of fluid past the tracheal tube cuff in a benchtop model. Br J Anaesth 78:557–562
Nathens AB, Marshall JC (1999) Selective decontamination of the digestive tract in surgical patients: a systematic review of the evidence. Arch Surg 134:170–176
Bonten MJ (2003) Prevention of hospital-acquired pneumonia: European perspective. Infect Dis Clin North Am17:773–784
Scannapieco FA, Rethman MP (2003) The relationship between periodontal diseases and respiratory diseases. Dent Today 22:79–83
Yoneyama T, Yoshida M, Ohrui T, Mukaiyama H, Okamoto H, Hoshiba K, Ihara S, Yanagisawa S, Ariumi S, Morita T, Mizuno Y, Ohsawa T, Akagawa Y, Hashimoto K, Sasaki H; Oral Care Working Group (2002) Oral care reduces pneumonia in older patients in nursing homes. J Am Geriatr Soc 50:430–433
Caton JG, Blieden TM, Lowenguth RA, Frantz BJ, Wagener CJ, Doblin JM, Stein SH, Proskin HM (1993) Comparison between mechanical cleaning and an antimicrobial rinse for the treatment and prevention of interdental gingivitis. J Clin Periodontol 20:172–178
Drakulovic MB, Bauer TT, Torres (1999) Supine body position as a risk factor for nosocomial pneumonia in mechanically ventilated patients: a randomised trial. Lancet 354:1851–1858
Smulders K, van der Hoeven H, Weers-Pothoff I, et al. (2002) A randomized clinical trial of intermittent subglottic secretion drainage in patients receiving mechanical ventilation. Chest 121:858–862
Combes P, Fauvage B, Oleyer C (2000) Nosocomial pneumonia in mechanically ventilated patients, a prospective randomised evaluation of the Stericath closed suctioning system. Intensive Care Med. 26:878–882
Cook DJ, Reeve BK, Guyatt GH (1996) Stress ulcer prophylaxis in critically ill patients. Resolving discordant meta-analyses. JAMA 275:308–314
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mori, H., Hirasawa, H., Oda, S. et al. Oral Care Reduces Incidence of Ventilator-Associated Pneumonia in ICU Populations. Intensive Care Med 32, 230–236 (2006). https://doi.org/10.1007/s00134-005-0014-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-0014-4