Abstract
Objective
To assess on a multinational level the prevalence and corresponding factors of selected unintended events that compromise patient safety (sentinel events) in intensive care units (ICUs).
Design
An observational, 24-h cross-sectional study of incidents in five representative categories.
Setting
205 ICUs worldwide
Measurements
Events were reported by intensive care unit staff members with the use of a structured questionnaire. Both ICU- and patient-related factors were assessed.
Results
In 1,913 adult patients a total of 584 events affecting 391 patients were reported. During 24 h multiple errors related to medication occurred in 136 patients; unplanned dislodgement or inappropriate disconnection of lines, catheters, and drains in 158; equipment failure in 112; loss, obstruction or leakage of artificial airway in 47; and inappropriate turn-off of alarms in 17. Per 100 patient days, 38.8 (95% confidence interval 34.7–42.9) events were observed. In a multiple logistic regression with ICU as a random component, the following were associated with elevated odds for experiencing a sentinel event: any organ failure (odds ratio 1.13, 95% confidence interval 1.00–1.28), a higher intensity in level of care (odds ratio 1.62, 95% confidence interval 1.18–2.22), and time of exposure (odds ratio 1.06, 95% confidence interval 1.04–1.08).
Conclusions
Sentinel events related to medication, indwelling lines, airway, and equipment failure in ICUs occur with considerable frequency. Although patient safety is recognised as a serious issue in many ICUs, there is an urgent need for development and implementation of strategies for prevention and early detection of errors.
Similar content being viewed by others
Introduction
Patient safety has achieved a high priority in many health care systems since the report by the Institute of Medicine in the USA [1] and publication in other countries [2, 3, 4, 5]. Patient safety is the attempt to assure that a course of medical treatment will proceed correctly and provide the best possible chance to achieve a desired outcome. Patient safety is therefore an essential component in the practice of intensive care medicine. However, it seems that the complexity of processes and medical conditions dealt with in intensive care units (ICUs) makes the system vulnerable and prone to error [6]. Because the close monitoring and supervision typical of ICU environments offer an ideal opportunity to detect errors and their contributing factors, there is a growing body of literature on several types of unintended events in ICUs [7, 8, 9]. Nearly all existing reports are based on observations in single ICUs or in relatively small national samples [10, 11, 12, 13]. Consequently, two important questions have not yet been answered: Is there a general pattern of error susceptibility in ICUs? If so, what is the prevalence of important types of errors in this setting?
We conducted a prospective, observational, multinational study on the prevalence of selected unintended events in intensive care medicine. A cross-sectional design with a 24-h observation period was chosen to ensure a concentrated effort on data collection. In addition, we assessed the impact of several ICU- and patient-related factors, such as workload of medical personnel and severity of illness, on the frequency and types of selected unintended events.
Methods
The Sentinel Events Evaluation (SEE) study was conducted by the Research Group on Quality Improvement of the European Society of Intensive Care Medicine (ESICM) in association with the Section on Health Services Research and Outcome. The study was endorsed by the European Critical Care Research Network. After an announcement and call for participants, 280 ICUs registered for the study by December 2003. During the registration process, the date of the study — January 21, 2004 — with its limited 24-h observation period was communicated to all participants. Ultimately, 220 ICUs from 29 countries and four continents participated.
Because the study was observational and no additional interventions were performed, the need for informed consent was waived by the institutional review board. Each ICU, however, was made responsible for obtaining local permissions as necessary.
Definition and assessment of sentinel events
A sentinel event was defined as an occurrence that harmed or could have harmed a patient. We looked at selected unintended events within the following categories: (1) medication (wrong dose, drug, route); (2) airway (unplanned extubation, artificial airway obstruction, cuff leakage prompting reintubation); (3) indwelling lines (intravascular cannulas and the attached fluid delivery sets), catheters, probes and drains (unplanned dislodgement, inappropriate disconnection); (4) equipment failure (infusion devices, ventilator and accessories, renal replacement devices, power and oxygen supply); and (5) alarms (inappropriate turn-off).
All nurses and physicians on duty in the participating ICUs during the 24-h study period were requested to answer a questionnaire available at the bedside of each patient. The questionnaire asked in a structured form whether and at which time any of the selected sentinel events had happened. In addition the utilisation of devices that could lead to the occurrence of selected sentinel events (e.g. use of several lines, drains, catheters) was assessed (see electronic supplementary material). An ICU coordinator in each participating ICU was responsible for the briefing of the ICU team, data collection and transmission. His or her obligations included the provision of information regarding ICU characteristics and classification of severity of illness and medical personnel workload for every patient. Data acquisition and reporting were anonymous for both patients and medical personnel.
Patient sample
The study included all patients staying in the participating ICUs, including patients admitted or discharged, during the 24-h study period.
Patient-related factors
For individual patients, the medical personnel recorded age, sex, time of ICU admission and discharge, and frequency, characteristics and time of the predefined unintended events. To facilitate reporting without the fear of blame there was no collection of any information regarding the outcome of unintended events.
To determine the severity of illness in every patient, the items necessary for calculating the Sequential Organ Failure Assessment (SOFA) score (to quantify the presence and degree of organ dysfunction/failure and consequently provide a surrogate for severity of illness) were collected [14], and all items for the Nine Equivalents of Nursing Manpower Use Score (NEMS) were also recorded (as a surrogate marker for the amount of nursing workload use and consequently of the level of care provided to each patient) [15]. The duration of each patient's stay in the ICU before and during the 24-h observation period was calculated from the time of admission to the time of discharge and is reported as “ICU length of stay before observation” (days) and “risk time” (hours), respectively.
ICU-related factors
For every ICU the following characteristics were recorded: hospital size, ICU type and size, shift schedule for nurses and physicians, number of nurses and physicians appointed to each specific shift, number of occupied and free beds in each shift, maximum number of patients in each shift and number of admitted and discharged patients in each shift. These data allowed us to calculate occupancy rate, patient-to-nurse ratio and patient-to-physician ratio for each shift and each ICU. Information about any existing system for formal critical incident reporting was also recorded.
Database and data collection
Patient data were recorded using a dedicated project website and online data collection software. The website contained (1) all documentation, including detailed definitions of all data fields and events (see electronic supplementary material); (2) data collection sheets available for download; and (3) access to the study database with its data entry forms.
To ensure consistent quality of the data in ICUs from different participating countries, the questionnaires were available in six languages: English, German, Italian, French, Portuguese, and Spanish (see electronic supplementary material).
Data collected from each ICU were entered into the study database by the appointed ICU coordinator. ICU coordinators who could not use the online data entry forms (e.g. because of a poor or nonexistent Internet connection) were allowed to submit paper data sheets to the project center (n = 12 ICUs). These data were entered into the online database system by project personnel.
During data entry by ICU coordinators or project personnel, plausibility and completeness checks were performed online. Each variable was defined in detail before the start of data collection, and the definitions were available in both paper and electronic form. To facilitate plausibility checking, each variable was assigned a range of probable values and a range of possible values (storage range).
Data collection started at the beginning of the nurses' day shift. The study period was designed to overlap a second day (but not to exceed 24 h) to be sure that data acquisition in each ICU included at least one day shift and one night shift.
Statistical analysis
Statistical analysis was performed using the SAS system, version 8.02 (SAS Institute, Cary, NC). Either the number of all patients in the final study sample, the number of patients exposed to a specific item, the number of all ICUs contributing patients to the final study sample, or the number of patient days (calculated as total hours at risk for all patients, divided by 24) served as denominator. The number of patients suffering an event or the number of events in total or in different categories served as numerator.
We calculated odds ratios for the risk of experiencing an unintended event at least once during the observation period. In a first step, multilevel logistic regression with ICU as a random component was applied separately per factor using linear and, if appropriate, quadratic terms to investigate the influence of all factors assessed as patient related. The same univariate model was applied to assess the influence of all collected ICU-related factors. Smoothed distribution graphs for the event probability were used to clarify the form of the univariate dependencies. Finally, a multiple logistic regression with backward elimination and ICU as a random component was performed. We included influence variables significant in the univariate logistic regression, eliminating a few of these variables due to high correlations with the others.
Unless otherwise specified, results are expressed as median (1st – 3rd quartile). All P values are based on two-tailed tests of significance. A P value of < 0.05 was considered significant.
Results
ICU and patient sample
After exclusion of 173 patients aged < 18 years the final study sample consisted of 1,913 adult patients (61% men) from 205 ICUs and 29 countries (Table 1). The mean age was 62.3 (± 16.3 standard deviation; range 18–99) years. Median ICU length of stay before observation was 2.8 days (quartiles 0.5–11.2). The median SOFA score was 4 (quartiles 2–7). The observed risk time (actual time of a patient within the ICU during the observation period) ranged from 0.5 to 24 h, median 24.0 (quartiles 15.0–24.0). The median NEMS was 27 (quartiles 18–38).
The majority of the 205 ICUs in the final study sample were of a mixed type (n = 143); the remaining ICUs were described as surgical (n = 24), medical (n = 19), trauma (n = 9) or other (n = 8). The ICUs were located in hospitals with < 300 beds (20%), 300–600 beds (44%) or > 600 beds (36%). The ICUs had a capacity of < 7 beds (19%), 7–12 beds (58%) or > 12 beds (23%). Most ICUs were organised with three nurse shifts (70%) and two (52%) or three (48%) physician shifts per day. The median patient-to-nurse ratio ranged from 1.3 (shift 1) to 2.0 (shift 3), and the median patient-to-physician ratio ranged from 3.0 (shift 1) to 6.0 (shift 3). In 39% of the ICUs included in the final study sample, an existing system for formal critical incident reporting was in use.
Occurrence and type of sentinel events
In the 1,913 patients, 584 sentinel events affecting 391 patients were reported for the 24-hour study period. Most (1,522) patients experienced no event, 268 patients experienced only 1 event, and 123 patients experienced > 1 event. Fifty-five (27%) of the 205 ICUs reported no sentinel events.
In total, 38.8 (95% confidence interval 34.7–42.9) events per 100 patient days were observed. Table 2 gives the corresponding numbers for all event categories. There was no noticeable difference in the number of events per 100 patient days between ICUs with or without an existing incident reporting system in use.
Within the five selected categories, the most frequent events were related to lines, catheters and drains, and occurred in 158 patients (Table 3). Events associated with the prescription (74 patients) or administration (62 patients) of drugs were the second most frequent observation: drug administration errors included a wrong drug in 15 patients, a wrong dose in 38 patients and a wrong route in 9 patients. The most frequent equipment failure was related to infusion devices (n = 37), followed by failure or dysfunction of ventilators (n = 20; occurred in 1.9% of all patients receiving mechanical ventilation) or of renal replacement devices (n = 12; occurred in 8.5% of all patients receiving renal replacement therapies). Failure of power or oxygen supply at the patient's bedside was reported in 20 and 9 cases, respectively. An unplanned extubation occurred in 12 of the 1,627 patients with an endotracheal tube or cannula in use, and an artificial airway obstruction or cuff leakage occurred in 23 and 13 patients, respectively. An inappropriate turn-off of alarms was reported on 17 occasions. Only one of these 17 occurrences was related to a corresponding event from another category (failure of oxygen supply).
Predictors of sentinel events
An univariate analysis showed that a higher severity of illness, a higher level of care, a longer length of stay in the ICU before observation, and a longer duration of exposure (risk time) were associated with elevated odds for experiencing a sentinel event (Table 4).
With respect to ICU-related variables, the univariate analysis showed an association of trauma ICUs with lower odds for the occurrence of sentinel events (odds ratio 0.47, 95% confidence interval 0.22–1.00; P = 0.04). The patient-to-nurse ratio exhibited a slight nonlinear influence (because of that nonlinearity, it has no overall odds ratio; linear term P = 0.02, quadratic term P = 0.006), as did the number of admissions and discharges (linear term P = 0.04, quadratic term P = 0.003). No other ICU-related variables were significantly associated with the occurrence of sentinel events.
In a stepwise multiple logistic regression analysis with ICUs as a random factor and backward elimination, one ICU-related and three patient-related variables remained in the final model (Table 5). Of note, this advanced statistical model explains only 11% of the observed variations, of which 5% are contributed by the remaining variability on ICU level.
Discussion
The results of the SEE multinational study confirm previous findings from single institutions showing that patients in ICUs are frequently exposed to errors [6, 7, 8, 9, 10, 11, 12]. For five selected categories of intensive care management, we found a total prevalence of 38.8 unintended events per 100 patient days. Considering that this number, derived from self-reports, may underestimate the frequency of errors, these results may be of even greater clinical relevance. ICUs have been developed to provide optimal care for patients at risk from several medical conditions, but it turns out that this particular clinical environment, like other hospital areas, carries its own risks [16]. The SEE study demonstrates that these weak points in patient safety are not attributable to suboptimal care in a few individual ICUs but represent a common pattern. Considering the complexity of highly developed intensive care, this is not surprising. In their landmark study in 1995, Donchin et al. reported an average of 178 daily activities in intensive care patients; this number may have increased since that report was released [6].
Furthermore, intensive care is characterised by a complex course of interaction among several medical specialties [17]. One important example of this interaction is the process of prescribing and administering drugs. In the SEE study we found a nearly equal prevalence of errors in prescription and administration of drugs, resulting in 10.5 events per 100 patient days. This observation is in line with reports from several single ICUs [18, 19, 20, 21, 22] and highlights an area of risk for potential patient harm. In one study, 20% of medication errors at the administration stage were considered potentially life-threatening [18].
Another area with a high potential for patient harm is the management of artificial airways [23, 24]. In addition to possible immediately life-threatening complications, at least one study has shown that unplanned extubations are associated with prolonged mechanical ventilation, longer ICU and hospital stay and increased need for chronic care [25]. The authors reported 1.6 unplanned extubations per 100 days of intubation. This number corresponds fairly well to our event rate of 0.7% unplanned extubations.
The most frequent occurrences were related to the unplanned dislodgement or inappropriate disconnection of lines, drains and catheters. Both types of unintended events have the potential for considerable harm [26]. Although the unintended removal of a Foley catheter or an enteral nutrition probe might be seen as a small misadventure, even these minor events could lead to urinary tract bleeding or aspiration of gastric content. In contrast, the risks associated with the dislodgement and disconnection of dialysis catheters are evident, and a prevalence of 3.8% and 1.9%, respectively, in our study should be noted with concern [27, 28].
Intensive care depends on the stable functioning of technical equipment. Our results show, for the first time in a large, multinational sample of ICUs, that technical failures frequently lead to events that compromise patient safety. This conclusion is in keeping with an analysis of 1,004 reports to French authorities of incidents involving medical devices in anaesthesia and intensive care that revealed 12 deaths attributable to the failure of a device [29].
As would be expected, univariate and multivariate analysis in our study showed that patients who are more severely ill and who receive a higher level of care are more likely to experience an unintended event. This finding directly reflects the complexity of care of these patients. Less clear was the analysis of ICU-related factors. Our observational study did not demonstrate a noticeable impact of the observed system-based factors on the occurrence of errors. The only significant variable, “patient-to-nurse ratio”, had a small effect with a surprising tendency for lower odds at low and high levels. A small range of the median patient-to-nurse ratio (1.3–2.0) and complex interactions with other ICU-related or unmeasured factors (e.g. sedation levels) as well as hidden causes may have contributed to this finding. Even more, it represents only a negligible part of the variation (0.6%) and might be a chance finding due to multiple testing.
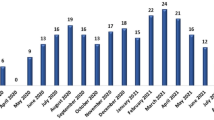
In our multivariate model, the most pronounced effect was seen when ICUs were included as random components. This effect should be noted, but this sophisticated statistical model has little explanatory power. One reason might be that components that have been shown to influence the occurrence of errors, such as variations in ICU organisation [20], different formats of communication [30] and different cultures of communication [6] are difficult to measure and were outside the scope of our 24-h observation. Obviously another taxonomy [31] of contributing factors would have identified different contextual information. But even a simple chronological plot of the frequency of events (Fig. 1) reveals a pattern that is probably associated with several courses of action (e.g. rounds, shift changes) during daily ICU operation. Donchin et al. reported a similar diurnal distribution of critical incidents corresponding to physicians' and nurses' morning peak activities and the times of the nurses' shift changes [6].
Other limitations of our study relate mainly to methodological questions. First, in order to facilitate reporting without any fear of blame we did not collect information regarding actual patient harm. Therefore it is not possible to draw any conclusions about the impact of unintended events on patients outcome. Second, our study focused on events related to errors of commission and did not record errors of omission. Third, we did not collect data about the use and impact of electronic medication prescribing systems, but with its growing propagation this technology becomes an area for further research. Finally, it is important to acknowledge several problems in measuring errors. Different formats of data collection like chart review or incident reporting will lead to different findings [32]. Using external observers might be considered as “gold standard” but is heavily resource consuming and implements the bias of different behaviour under observation (Hawthorne effect). In contrast, as shown by several authors, a self-reporting method carries the risk of under-reporting [6, 33, 34]. Because we used a facilitated reporting by a structured questionnaire for the occurrence of selected events in a short period of time, we are confident that this problem was minimised. Finally, in our surveillance the possibility of volunteer bias needs to be considered for the ICUs electing to join the study.
Results from the SEE study suggest an urgent need for ICUs to improve the safety of medication prescription and administration and the appropriate maintenance of indwelling lines, catheters, drains and airways, as well as to improve the development of error-free, stable technical equipment. Apart from the findings we have reported, the most remarkable aspect of the SEE study was the eagerness of a large number of ICU personnel worldwide to participate. The intensive care community has proved that patient safety is recognised as a top-priority issue and demonstrated that open communication is the starting point for addressing flaws in our current system of intensive care.
References
Kohn LT, Corrigan KM, Donaldson MS, (eds) (1999) To err is human: building a safer health system. Washington DC, National Academy Press
Altman DE, Clancy C, Blendon RJ (2004) Improving patient safety – five years after the IOM report. New Engl J Med 351:2041–2043
Wilson RM, Runciman WB, Gibberd RW, Harrison B (1995) The quality in Australian health care study. Med J Aust 163:458–471
Vincent C, Neale G, Woloshynowych M (2001) Adverse Events in British hospitals: preliminary retrospective record review. BMJ 322:517–519
Schioler T, Lipczak H, Pedersen BL, Morgensen TS, Bech KB, Stockmarr A, Svenning AR, Frolich A (2001) Forekomsten af utilsigtede haendelser pa sygehuse. En retrospektiv gennemgang af journaler. Ugeskr Laeger 163:5370–5378
Donchin Y, Gopher D, Olin M, Badihi Y, Biesky M, Sprung CL, Pizov R, Cotev S (1995) A look into the nature and causes of human errors in the intensive care unit. Crit Care Med 23:294–300
Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, Lilly CM, Stone PH, Lockley SW, Bates DW, Czeisler CA (2004) Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med 351:1838–1848
Flaatten H, Hevroy O (1999) Errors in the intensive care unit (ICU). Experiences with an anonymous registration. Acta Anaesthesiol Scand 43:614–617
Buckley TA, Short TG, Rowbottom YM, Oh TE (1997) Critical incident reporting in the intensive care unit. Anaesthesia 52:403–409
Bracco D, Favre JB, Bissonnette B, Wasserfallen JB, Revelly JP, Ravussin P, Chiolero R (2001) Human errors in a multidisciplinary intensive care unit: a 1-year prospective study. Intensive Care Med 27:137–145
Osmon S, Carolyn BH, Dunagan CW, Prentice D, Fraser VJ, Kollef MH (2004) Reporting of medical errors: an intensive care unit experience. Crit Care Med 32:727–733
Beckmann U, Baldwin I, Hart GK, Runciman WB (1996) The Australian Incident Monitoring Study in Intensive Care: AIMS-ICU. An analysis of the first year of reporting. Anaesth Intensive Care 24:320–329
Wu AW, Pronovost P, Morlock L (2002) ICU incident reporting systems. J Crit Care 17:86–94
Vincent JL, Moreno R, Takala J, Willats S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Reis Miranda D, Moreno R, Iapichino G (1997) Nine equivalents of nursing manpower use score (NEMS). Intensive Care Med 23:760–765
Donchin Y, Seagull FJ (2002) The hostile environment of the intensive care unit. Curr Opin Crit Care 8:316–320
Dodek PM, Raboud J (2003) Explicit approach to rounds in an ICU improves communication and satisfaction of providers. Intensive Care Med 29:1584–1588
Tissot E, Cornette C, Demoly P, Jacquet M, Barale F, Capellier G (1999) Medication errors at the administration stage in an intensive care unit. Intensive Care Med 25:353–359
Calabrese AD, Erstad BL, Brandl K, Barletta JF, Kane SL, Sherman DS (2001) Medication administration errors in adult patients in the ICU. Intensive Care Med 27:1592–1598
van den Bemt PM, Fijn R, van der Voort PH, Gossen AA, Egberts TC, Brouwers JR (2002) Frequency and determinants of drug administration errors in the intensive care unit. Crit Care Med 30:846–850
Parshuram CS, Ng GY, Ho TK, Klein J, Moore AM, Bohn D, Koren G (2003) Discrepancies between ordered and delivered concentrations of opiate infusions in critical care. Crit Care Med 31:2483–2487
Herout PM, Erstad BL (2004) Medication errors involving continuously infused medications in a surgical intensive care unit. Crit Care Med 32:428–432
Kapadia FN, Bajan KB, Raje KV (2000) Airway accidents in intubated intensive care unit patients: an epidemiological study. Crit Care Med 28:659–664
Needham DM, Thompson DA, Holzmueller CG, Dorman T, Lubomski LH, Wu AW, Morlock LL, Pronovost PJ (2004) A system factors analysis of airway events from the Intensive Care Unit Safety Reporting System (ICUSRS). Crit Care Med 32:2227–2233
Epstein SK, Nevins ML, Chung J (2000) Effect of unplanned extubation on outcome of mechanical ventilation. Am J Respir Crit Care Med 161:1912–1916
Needham DM, Sinopoli DJ, Thompson DA, Holzmueller CG, Dorman T, Lubomski LH, Wu AW, Morlock LL, Makary MA, Pronovost PJ (2005) A system factors analysis of “line, tube, and drain” incidents in the intensive care unit. Crit Care Med 33:1701–1707
Pronovost PJ, Wu AW, Sexton JB (2004) Acute decompensation after removing a central line: practical approaches to increasing safety in the intensive care unit. Ann Intern Med 140:1025–1033
Ely EW, Hite RD, Baker AM, Johnson MM, Bowton DL, Haponik EF (1999) Venous air embolism from central venous catheterization: a need for increased physician awareness. Crit Care Med 27:2113–2117
Beydon L, Conreux F, Le Gall R, Safran D, Cazalaa JB (2001) Sous-commission de Materiovigilance for Anaesthesia and Intensive Care. Analysis of the French health ministry's national register of incidents involving medical devices in anaesthesia and intensive care. Br J Anaesth 86:382–387
Wasserfallen JB, Butschi AJ, Muff P, Biollaz J, Schaller MD, Pannatier A, Revelly JP, Chiolero R (2004) Format of medical order sheet improves security of antibiotics prescription: The experience of an intensive care unit. Crit Care Med 32:655–659
Chang A, Schyve PM, Croteau RJ, O'Leary DS, Loeb JM (2005) The JCAHO patient safety event taxonomy: a standardized terminology and classification schema for near misses and adverse events. Int J Qual Health Care 17:95–105
Beckmann U, Bohringer C, Carless R, Gillies DM, Runciman WB, Wu WA, Pronovost P (2003) Evaluation of two methods for quality improvement in intensive care: Faclitated incident monitoring and retrospective medical chart review. Crit Care Med 31:1006–1011
Vincent C, Stanhope N, Crowley-Murphy M (1999) Reasons for not reporting adverse incidents: an empirical study. J Eval Clin Pract 5:13–21
Stanhope N, Crowley-Murphy M, Vincent C, O'Connor AM, Taylor-Adams SE (1999) An evaluation of adverse incident reporting. J Eval Clin Pract 5:5–12
Acknowledgements
The SEE study was supported by the Austrian Center for Documentation and Quality Assurance in Intensive Care Medicine (ASDI) and endorsed by the European Critical Care Research Network (ECCRN) of the European Society of Intensive Care Medicine (ESICM). We are indebted to Mary McKenney for editorial advice and to Gerhard Krenn for programming the study website. We are most grateful to the staff of all the ICUs that contributed to the SEE study. A list of persons in charge of the study at the ICU level and their corresponding country is provided in the electronic supplementary material.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the Research Group on Quality Improvement of the European Society of Intensive Care Medicine (ESICM) and the SEE study investigators
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-006-0291-6
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Valentin, A., Capuzzo, M., Guidet, B. et al. Patient safety in intensive care: results from the multinational Sentinel Events Evaluation (SEE) study . Intensive Care Med 32, 1591–1598 (2006). https://doi.org/10.1007/s00134-006-0290-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0290-7