Abstract
BACKGROUND
The accuracy of information transferred during hand-offs is uncertain.
OBJECTIVE
To describe the frequency, types, and harm potential of medication discrepancies in resident-written sign-outs.
DESIGN
Retrospective cohort study.
PARTICIPANTS
Internal Medicine interns and their patients at a single hospital in January 2006.
MEASUREMENTS
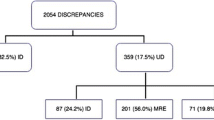
Daily written sign-outs were compared to daily medication lists in patient charts (gold standard). Medication discrepancies were labeled omissions (medication in chart, but not on sign-out) or commissions (medication on sign-out, but not in chart). Discrepancies were also classified as index errors (the first time an error was made) and the proportion of index errors that persisted on subsequent days. Using a modified classification scheme, discrepancies were rated as having minimal, moderate, or severe potential to harm.
RESULTS
One hundred eighty-six of 247 (75%) patients and 10 of 10(100%) interns consented. In the 165 (89%) patients’ charts abstracted and compared with the sign-out, there were 1,876 of 6,942 (27%) medication chart entries that were discrepant with the sign-out with 80% (1,490/1,876) labeled omissions. These discrepancies originated from 758 index errors, of which 63% (481) persisted past the first day. Omissions were more likely to persist than commissions (68% [382 of 580] vs 53% [99 of 188], p < .001). Greater than half (54%) of index discrepancies were moderate or severely harmful. Although omissions were more frequent, commissions were more likely to be severely harmful (38% [72 of 188] vs 11% [65 of 580], p < .0001).
CONCLUSIONS
Written sign-outs contain potentially harmful medication discrepancies. Whereas linking sign-outs to electronic medical records can address this problem, current efforts should also emphasize the importance of vigilant updating in the many hospitals without this technology.
Similar content being viewed by others
References
Solet DJ, Norvell JM, Rutan GH, Frankel RM. Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med. 2005;80(12):1094–99.
Arora V, Johnson J, Lovinger D, Humphrey H, Meltzer D. Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005;14:401–7.
Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: Results of a trial of hospitalists. Ann Intern Med. 2002;137(11):866–74.
Arora V, Dunphy C, Chang VY, et al. The effects of on-duty napping on intern sleep time and fatigue. Ann Intern Med. 2006;144(11):792–8.
Franke RH, Kaul JD. The Hawthorne experiments: first statistical interpretation. Am Sociol Rev. 1978;43:623–43.
Cornish P, Knowles S, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med 2005;165:424–9.
Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc. 2006;13(5):547–56.
Glucose Roller Coaster. AHRQ Web M&M. http://www.webmm.ahrq.gov/case.aspx?caseID=70. Accessed August 27, 2007.
Bates DW, Cohen M, Leape LL, et al. Reducing the frequency of errors in medicine using information technology. J Am Med Inform Assoc. 2001;8(4):299–308.
Edwards M, Moczygemba J. Reducing medical errors through better documentation. Health Care Manag. 2004;23(4):329–33.
Van Eaton EG, Horvath KD, Lober WB, Pellegrini CA. Organizing the transfer of patient care information: the development of a computerized resident sign-out system. Surgery. 2004;136(1):5–13.
Van Eaton EG, Horvath KD, Lober WB, Rossini AJ, Pellegrini CA. A randomized, controlled trial evaluating the impact of a computerized rounding and sign-out system on continuity of care and resident work hours. J Am Coll Surg. 2005;200(4):538–45.
Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293(10):1197–203.
Horwitz LI, Krumholz HM, Green ML, Huot SJ. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med. 2006;166:1173–7.
Arora V, Johnson J. A model for building a standardized hand-off protocol. Jt Comm J Qual Patient Saf. 2006;32(11):646–55.
Vidyarthi AR, Arora V, Schnipper JL, Wall SD, Wachter RM. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1(4):257–66.
Acknowledgments
We are grateful to Ms. Kimberly Alvarez and Mr. Micah Prochaska for their assistance in manuscript preparation and research assistance. We acknowledge funding from the Pritzker Summer Research Program, the Hartford Health Outcomes Research Scholars Program, the Donald W. Reynolds Foundation, and the National Institute of General Medical Sciences. Prior presentations of this work include the Chicago Patient Safety Forum in March 2007, the University of Chicago Medical Education Day in April 2007, and the Society of Hospital Medicine Annual Meeting in Dallas, TX in May 2007.
Conflict of Interest
Dr. Vineet Arora, Julia Kao, Dr. David Lovinger, and Dr. Samuel Seiden have no potential conflicts of interests. Potential conflicts of interest exist with Dr. David Meltzer with the following: National Institute of Health, Centers for Disease Control, Robert Wood Johnson Foundation, Pfizer, Merck, Lilly, Juvenile Diabetes Research Foundation, InHealth, and PeopleChart.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arora, V., Kao, J., Lovinger, D. et al. Medication Discrepancies in Resident Sign-Outs and Their Potential to Harm. J GEN INTERN MED 22, 1751–1755 (2007). https://doi.org/10.1007/s11606-007-0415-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-007-0415-x