ABSTRACT
BACKGROUND
Physicians are under increased pressure to help control rising health care costs, though they lack information regarding cost implications of patient care decisions.
OBJECTIVE
To evaluate the impact of real-time display of laboratory costs on primary care physician ordering of common laboratory tests in the outpatient setting.
DESIGN
Interrupted time series analysis with a parallel control group.
PARTICIPANTS
Two hundred and fifteen primary care physicians (153 intervention and 62 control) using a common electronic health record between April 2010 and November 2011. The setting was an alliance of five multispecialty group practices in Massachusetts.
INTERVENTION
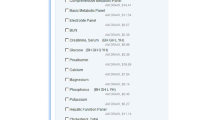
The average Medicare reimbursement rate for 27 laboratory tests was displayed within an electronic health record at the time of ordering, including 21 lower cost tests (< $40.00) and six higher cost tests (> $40.00).
MAIN MEASURES
We compared the change-in-slope of the monthly laboratory ordering rate between intervention and control physicians for 12 months pre-intervention and 6 months post-intervention. We surveyed all intervention and control physicians at 6 months post-intervention to assess attitudes regarding costs and cost displays.
KEY RESULTS
Among 27 laboratory tests, intervention physicians demonstrated a significant decrease in ordering rates compared to control physicians for five (19 %) tests. This included a significant relative decrease in ordering rates for four of 21 (19 %) lower cost laboratory tests and one of six (17 %) higher cost laboratory tests. A majority (81 %) of physicians reported that the intervention improved their knowledge of the relative costs of laboratory tests.
CONCLUSIONS
Real-time display of cost information in an electronic health record can lead to a modest reduction in ordering of laboratory tests, and is well received. Our study demonstrates that electronic health records can serve as a tool to promote cost transparency and reduce laboratory test use.

Similar content being viewed by others
REFERENCES
Owens DK, Qaseem A, Chou R, Shekelle P. High-value, cost-conscious health care: concepts for clinicians to evaluate the benefits, harms, and costs of medical interventions. Ann Intern Med. 2011;154(3):174–180.
Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273–287.
Stremikis K, Schoen C, Fryer A-K. A Call for Change: The 2011 Commonwealth Fund Survey of Public Views of the U.S. Health System. Issue Brief, The Commonwealth Fund. 2011; 6:1–23.
The Commonwealth Fund Commission. The Commonwealth Fund Commission on a High Performance Health System, Why Not the Best? Results from the National Scorecard on U.S. Health System Performance, 2008. The Commonwealth Fund. 2008;97:1–60.
Qaseem A, Alguire P, Dallas P, Feinberg LE, Fitzgerald FT, Horwitch C, et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012;156(2):147.
Chernew ME, Mechanic RE, Landon BE, Safran DG. Private-payer innovation in Massachusetts: the ‘alternative quality contract’. Health Aff (Millwood). 2011;30(1):51–61.
Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care–two essential elements of delivery-system reform. N Engl J Med. 2009;361(24):2301–2303.
Institute of Medicine. Best care at lower cost: The path to continuously learning health care in America. Washington DC: The National Academies Press; 2012.
Korenstein D, Falk R, Howell EA, Bishop T, Keyhani S. Overuse of health care services in the United States: an understudied problem. Arch Intern Med. 2012;172(2):171–178.
Alexander GC, Casalino LP, Tseng CW, McFadden D, Meltzer DO. Barriers to patient-physician communication about out-of-pocket costs. J Gen Intern Med. 2004;19(8):856–860.
Alexander GC, Casalino LP, Meltzer DO. Patient-physician communication about out-of-pocket costs. JAMA. 2003;290(7):953–958.
Mallya G, Pollack CE, Polsky D. Are primary care physicians ready to practice in a consumer-driven environment? Am J Manag Care. 2008;14(10):661–668.
Pham HH, Alexander GC, O’Malley AS. Physician consideration of patients’ out-of-pocket costs in making common clinical decisions. Arch Intern Med. 2007;167(7):663–668.
Tilburt JC, Wynia MK, Sheeler RD, et al. VIews of us physicians about controlling health care costs. JAMA. 2013;310(4):380–388.
Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–752.
Blumenthal D. Implementation of the federal health information technology initiative. N Engl J Med. 2011;365(25):2426–2431.
Sequist TD, Fitzmaurice GM, Marshall R, Shaykevich S, Marston A, Safran DG, et al. Cultural competency training and performance reports to improve diabetes care for black patients: a cluster randomized, controlled trial. Ann Intern Med. 2010;152(1):40–46.
Sequist TD, Marshall R, Lampert S, Buechler EJ, Lee TH. Missed opportunities in the primary care management of early acute ischemic heart disease. Arch Intern Med. 2006;166(20):2237–2243.
Sequist TD, Schneider EC, Anastario M, Odigie EG, Marshall R, Rogers WH, et al. Quality monitoring of physicians: linking patients’ experiences of care to clinical quality and outcomes. J Gen Intern Med. 2008;23(11):1784–1790.
Sequist TD, Zaslavsky AM, Marshall R, Fletcher RH, Ayanian JZ. Patient and physician reminders to promote colorectal cancer screening: a randomized controlled trial. Arch Intern Med. 2009;169(4):364–371.
Ginsburg ME, Kravitz RL, Sandberg WA. A survey of physician attitudes and practices concerning cost-effectiveness in patient care. West J Med. 2000;173(6):390–394.
Hampers LC, Cha S, Gutglass DJ, Krug SE, Binns HJ. The effect of price information on test-ordering behavior and patient outcomes in a pediatric emergency department. Pediatrics. 1999;103(4 Pt 2):877–882.
Tierney WM, Miller ME, McDonald CJ. The effect on test ordering of informing physicians of the charges for outpatient diagnostic tests. N Engl J Med. 1990;322(21):1499–1504.
Bates DW, Kuperman GJ, Jha A, Teich JM, Orav EJ, Ma’luf N, et al. Does the computerized display of charges affect inpatient ancillary test utilization? Arch Intern Med. 1997;157(21):2501–2508.
Durand DJ, Feldman LS, Lewin JS, Brotman DJ. Provider cost transparency alone has no impact on inpatient imaging utilization. J Am Coll Radiol. 2012. doi:10.1016/j.jacr.2012.06.020.
Feldman LS, Shihab HM, Thiemann D, Yeh HC, Ardolino M, Mandell S, et al. Impact of providing fee data on laboratory test ordering: a controlled clinical trial. JAMA Intern Med. 2013;173(10):903–908.
Calderon-Margalit R, Mor-Yosef S, Mayer M, Adler B, Shapira SC. An administrative intervention to improve the utilization of laboratory tests within a university hospital. Int J Qual Health Care. 2005;17(3):243–248.
Gama R, Nightingale PG, Broughton PM, Peters M, Ratcliffe JG, Bradby GV, et al. Modifying the request behaviour of clinicians. J Clin Pathol. 1992;45(3):248–249.
Sommers BD, Desai N, Fiskio J, Licurse A, Thorndike M, Katz JT, et al. An educational intervention to improve cost-effective care among medicine housestaff: a randomized controlled trial. Acad Med. 2012. doi:10.1097/ACM.0b013e31825373b3.
Stuebing EA, Miner TJ. Surgical vampires and rising health care expenditure: reducing the cost of daily phlebotomy. Arch Surg. 2011;146(5):524–527.
Bunting PS, Van Walraven C. Effect of a controlled feedback intervention on laboratory test ordering by community physicians. Clin Chem. 2004;50(2):321–326.
Sinaiko AD, Rosenthal MB. Increased price transparency in health care–challenges and potential effects. N Engl J Med. 2011;364(10):891–894.
Volpp KG, Loewenstein G, Asch DA. Assessing value in health care programs. JAMA. 2012;307(20):2153–2154.
Acknowledgements
We thank Shane Morong, BA for assistance with survey distribution and survey data acquisition and analysis.
Funding/Support
This study was not funded by any outside sponsors.
Prior Presentations
A portion of this data was presented as a plenary talk at the Society for General Internal Medicine Annual Meeting in Orlando, Florida on May 12, 2012.
Thomas D. Sequist had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of Interest Disclosures
The authors declare that they do not have any conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
Rights and permissions
About this article
Cite this article
Horn, D.M., Koplan, K.E., Senese, M.D. et al. The Impact of Cost Displays on Primary Care Physician Laboratory Test Ordering. J GEN INTERN MED 29, 708–714 (2014). https://doi.org/10.1007/s11606-013-2672-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-013-2672-1