Abstract
BACKGROUND: Internal medicine residents must be competent in advanced cardiac life support (ACLS) for board certification.
OBJECTIVE: To use a medical simulator to assess postgraduate year 2 (PGY-2) residents’ baseline proficiency in ACLS scenarios and evaluate the impact of an educational intervention grounded in deliberate practice on skill development to mastery standards.
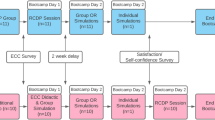
DESIGN: Pretest-posttest design without control group. After baseline evaluation, residents received 4, 2-hour ACLS education sessions using a medical simulator. Residents were then retested. Residents who did not achieve a research-derived minimum passing score (MPS) on each ACLS problem had more deliberate practice and were retested until the MPS was reached.
PARTICIPANTS: Forty-one PGY-2 internal medicine residents in a university-affiliated program.
MEASUREMENTS: Observational checklists based on American Heart Association (AHA) guidelines with interrater and internal consistency reliability estimates; deliberate practice time needed for residents to achieve minimum competency standards; demographics; United States Medical Licensing Examination Step 1 and Step 2 scores; and resident ratings of program quality and utility.
RESULTS: Performance improved significantly after simulator training. All residents met or exceeded the mastery competency standard. The amount of practice time needed to reach the MPS was a powerful (negative) predictor of posttest performance. The education program was rated highly.
CONCLUSIONS: A curriculum featuring deliberate practice dramatically increased the skills of residents in ACLS scenarios. Residents needed different amounts of training time to achieve minimum competency standards. Residents enjoy training, evaluation, and feedback in a simulated clinical environment. This mastery learning program and other competency-based efforts illustrate outcome-based medical education that is now prominent in accreditation reform of residency education.
Similar content being viewed by others
References
American Board of Internal Medicine. Requirements for certification in internal medicine. Available at: http://www.abim.org/cert/policiesim.shtm#6. Accessed July 7, 2005.
Cummins RO, Sanders A, Mancini E, Hazinski MF. In-hospital resuscitation: a statement for healthcare professionals from the American Heart Association Emergency Cardiac Care Committee and the Advanced Cardiac Life Support, Basic Life Support, Pediatric Resuscitation, and Program Administration Subcommittees. Circulation. 1997;95:2211–2.
Kaye W, Mancini ME, Rallis SF. Advanced cardiac life support refresher course using standardized objective-based mega code testing. Crit Care Med. 1987;15:55–60.
O’Steen DS, Kee CC, Minick MP. The retention of advanced cardiac life support knowledge among registered nurses. J Nurs Staff Dev. 1996;12:66–72.
Moser DK, Dracup K, Guzy PM, Taylor SE, Breu C. Cardiopulmonary resuscitation skills retention in family members of cardiac patients. Am J Emer Med. 1990;8:498–503.
Makker R, Gray-Siracusa K, Evers M. Evaluation of advanced cardiac life support in a community teaching hospital by use of actual cardiac arrests. Heart Lung. 1995;24:116–20.
Kaye W. Research on ACLS training—which methods improve skill and knowledge retention? Respir Care. 1995;40:538–46.
Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14,720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308.
Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293:305–10.
Issenberg SB, McGaghie WC, Hart IR, et al. Simulation technology for health care professional skills training and assessment. JAMA. 1999;282:861–6.
Dunn WF, ed. Simulators in Critical Care Education and Beyond. Des Plaines, IL: Society of Critical Care Medicine; 2004.
Tekian A, McGuire CH, McGaghie WC, eds. Innovative Simulations for Assessing Professional Competence. Chicago: Department of Medical Education, University of Illinois College of Medicine; 1999.
Gaba DM. Human work environment and simulators. In: Miller RD, ed. Anesthesia. 5th ed. Philadelphia: Churchill Livingstone; 2000:2613–68.
Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(suppl):S70–81.
Issenberg SB, McGaghie WC, Petrusa ER, Gordon DL, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27:10–28.
Boulet JR, Murray D, Kras J, et al. Reliability and validity of a simulation-based acute care skills assessment for medical students and residents. Anesthesiology. 2003;99:1270–80.
Issenberg SB, McGaghie WC, Gordon DL, et al. Effectiveness of a cardiology review course for internal medicine residents using simulation technology and deliberate practice. Teach Learn Med. 2002;14:223–8.
Ewy GA, Felner JM, Juul D, et al. Test of a cardiology patient simulator in fourth-year electives. J Med Educ. 1987;62:738–43.
Seymour NE, Gallagher AG, Roman SA, et al. Virtual reality training improves operating room performance. Ann Surg. 2002;236:458–64.
Bandura A. Self-Efficacy: The Exercise of Control. New York: W.H. Freeman; 1997.
Block JH, ed. Mastery Learning: Theory and Practice. New York: Holt, Rinehart and Winston; 1971.
McGaghia WC, Miller GE, Sajid A, Telder TV. Competency-Based Curriculum Development in Medical Education. Public Health Paper No. 68. Geneva, Switzerland: World Health Organization; 1978.
Carroll JB. A model of school learning. Teach Coll Rec. 1963;64:723–33.
Keller FS. “Good-bye, teacher ….” J Appl Behav Anal. 1968;1:79–89.
McClelland DC. Testing for competence rather than for “intelligence.” Am Psychol. 1973;28:1–14.
Bloom BS. Time and learning. Am Psychol. 1974;29:682–8.
Bloom BS. Human Characteristics and School Learning. New York: McGraw-Hill; 1976.
Kulik JA, Kulik C-LC, Cohen PA. A meta-analysis of outcome studies of Keller’s personalized system of instruction. Am Psychol. 1979;34:307–18.
Harden RM. Developments in outcome-based education. Med Teach. 2002;24:117–20.
Goroll AH, Sirio C, Duffy FD, et al. A new model for accreditation of residency programs in internal medicine. Ann Intern Med. 2004;140:902–9.
Wayne DB, Butter J, Siddall VJ, et al. Simulation-based training of internal medicine residents in advanced cardiac life support protocols: a randomized trial. Teach Learn Med. 2005;17:210–6.
Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston: Houghton Mifflin; 2002.
Cummins RO, ed. ACLS Provider Manual. Dallas: American Heart Association; 2001.
McGaghie WC, Renner BR, Kowlowitz V, et al. Development and evaluation of musculoskeletal performance measures for an objective structured clinical examination. Teach Learn Med. 1994;6:59–63.
Stufflebeam DL. The Checklists Development Checklist. Western Michigan University Evaluation Center, July 2000. Available at http://www.wmich.edu/evalctr/checklists/cdc.htm. Accessed 03/15/2005.
Wayne DB, Fudala MJ, Butter J, et al. Comparison of two standard setting methods for advanced cardiac life support training. Acad Med. 2005;80(suppl):S63-S66
Fleiss JL. Statistical Methods for Rates and Proportions. 2nd ed. New York: John Wiley & Sons; 1981.
Brennan RL, Prediger DJ. Coefficient kappa: some uses, misuses, and alternatives. Educ Psychol Meas. 1981;41:687–99.
Cortina JM. What is coefficient alpha? An examination of theory and applications. J Appl Psychol. 1993;78:93–104.
Samson GE, Graue ME, Weinstein T, Walberg HJ. Academic and occupational performance: a quantitative synthesis. Am Educ Res J. 1984;21:311–21.
Des Jarlias DC, Lyles C, Crepaz N, and the TREND Group. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004;94:361–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial Support: Excellence in Academic Medicine Act under the State of Illinois Department of Public Aid administered through Northwestern Memorial Hospital.
Rights and permissions
About this article
Cite this article
Wayne, D.B., Butter, J., Siddall, V.J. et al. Mastery learning of advanced cardiac life support skills by internal medicine residents using simulation technology and deliberate practice. J Gen Intern Med 21, 251–256 (2006). https://doi.org/10.1111/j.1525-1497.2006.00341.x
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1111/j.1525-1497.2006.00341.x